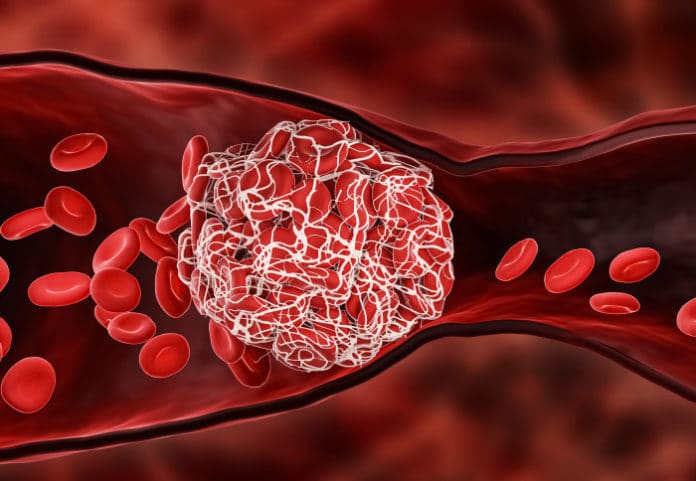
A blood clot is a clump of blood that can then leads to strokes and heart attacks. The condition can be treated with a clot-dissolving drug called tissue plasminogen activator (tPA). The drug disrupts the clots to clear the blocked blood vessel and re-establish blood flow.
Although, tPA has several side effects, including life-threatening and lasts only a few minutes in circulation. Repeated doses of it can lead to bleeding. Hence, it is used for a minority of potentially eligible patients.
Now, scientists at the Imperial College London have designed a drug delivery nanocapsule called tPA-cRGD-PEG-NV that could reduce the side effects of this blood clot-dissolving drug. They found that encasing tPA in newly designed tiny capsules can be targeted more specifically to harmful blood clots with increased circulation time.
Lead author Dr. Rongjun Chen of Imperial’s Department of Chemical Engineering said: “tPA has a narrow window between the desired effect and side effects, so we have wrapped it in a package that extends this therapeutic window and minimizes the required dose. Our results are exciting, but animal and clinical studies are required for validation.”
Blood clots consist of platelets that are bound together when activated. These platelets are held together with fibrinogen proteins that bind to activated platelets and form ‘bridges’ between them.
This new nanocapsule acts as a fibrinogen so that it seeks out clots within blood vessels. Scientists tested it on healthy human blood under both static conditions and physiological flow conditions. Under static conditions, blood was tested in Petri dishes, whereas in physiological flow conditions, blood was tested in a simulated blood vessel.
A computer model was designed to test flow conditions, where scientists simulated how the encapsulated tPA might act in circulating blood.
They found that the nanocapsules were highly selective in binding to activated platelets and that the time it took to dissolve clots was similar to that with unencapsulated tPA.
Co-corresponding author Professor Xiao Yun Xu of Imperial’s Department of Chemical Engineering said: “We combined experimental and computational work to characterize this nanocapsule. To build our computer model, we needed a mechanistic understanding of the interplay between the physical and biochemical processes. The model could be instrumental in animal and clinical trials of this potential nanomedicine, as well as in predicting optimal dosing for patients.”
“The purpose-built computer model was able to simulate nanocapsule transport to the clot site, its release of tPA, and its dissolution of clots. Our simulation illustrated the potential in predicting the outcome of blood clot treatments in clinically relevant scenarios.”
Co-author Professor Simon Thom of Imperial’s National Heart and Lung Institute said: “We’ve found a way to make a clot-busting drug more precisely targeted, potentially enhancing efficacy and reducing catastrophic side effects. This good work paves the way for safer delivery of drugs with otherwise harmful side effects and demonstrates the activity of nano-encapsulated tPA in a laboratory setting. Research is now needed in whole organisms to determine the capsule’s effectiveness in a more realistic setting.”
Journal Reference:
- Yu Huang et al. Fibrinogen-mimicking, multiarm nanovesicles for human thrombus-specific delivery of tissue plasminogen activator and targeted thrombolytic therapy. DOI: 10.1126/sciadv.abf9033