There are many types of cancer drugs to treat cancer. But, there is no way to discover how a patient will respond to a particular drug. So, MIT researchers have now come up with a new type of technique to predict how drugs will affect cancer cells taken from multiple myeloma patients.
Through this, they have shown that their predictions correlated with how those patients actually fared when treated with those cancer drugs.
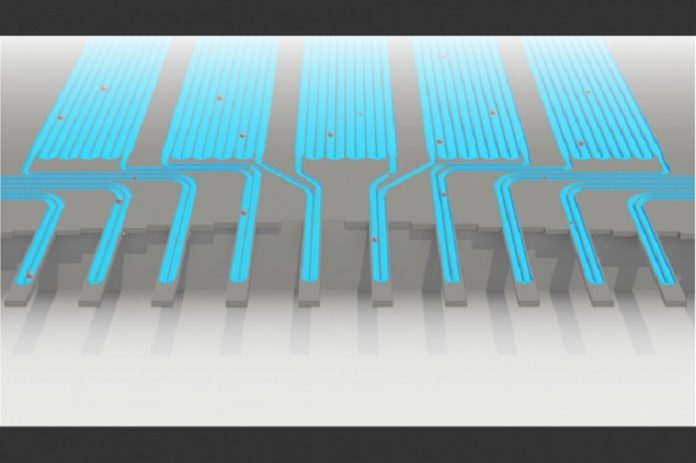
The technique basically relies on a previous technology that scientists had developed several years ago to weigh cells. Their device, known as a suspended microchannel resonator (SMR), can measure cell masses 10 to 100 times more accurately than any other technique.
Their new technique is the latest version of that device which can measure 50 to 100 cells per hour. It equipped with a series of SMR sensors that measure cells while flowing through tiny channels. Over a 20-minute period, each cell is weighed 10 times, which is enough to get an accurate MAR measurement.
Scott Manalis, the Andrew and Erna Viterbi Professor in the MIT departments of Biological Engineering and Mechanical Engineering said, “This type of testing could help doctors predict drug responses based on measurements of cancer cell growth rates after drug exposure.”
“For infectious diseases, antibiotic susceptibility testing based on cell proliferation has been extremely effective for many decades. Unlike bacteria, analogous tests for tumor cells have been challenging, in part because the cells don’t always proliferate upon removal from the patient. The measurement we developed doesn’t require proliferation.”
One of the difficulties while treating disease like myeloma is to choose the effective drug. Patients, for the most part, react well to the first round of treatment however in the long run backslide, and soon thereafter specialists must pick another medication. Notwithstanding, there is no real way to foresee which medication would be best for that specific patient around then.
During a session, scientists realize that their sensor would be utilized at the season of infection backslide, when the tumor may have created protection from particular treatments.
Mark Stevens, a visiting scientist at the Koch Institute said, “At this time of relapse, we would take a bone marrow biopsy from a patient, and we would test each therapy individually or in combinations that are typically used in the clinic. At that point, we’d be able to inform the clinician as to which therapy or combinations of therapies this patient seems to be most sensitive or most resistant to.”
According to scientists, their technique could efficiently screen myeloma cells for drug susceptibility. In addition, it could test many different drugs and drug combinations.
Andrew said, “This assay may fast-forward personalized medical care and the choice of effective therapies for myeloma both at diagnosis and at relapse. It may also be useful to profile susceptibility to minimal residual disease in order to further inform therapy and improve patient outcome.”